Compelling Clinical Data
ReActiv8 is the most thoroughly researched neuromodulation therapy for mechanical CLBP, globally.
Clinical Study Publications
RESTORE
- Prospective, randomized, controlled multi-center study comparing the effectiveness of ReActiv8 to Optimal Medical Management (OMM) for the treatment of intractable chronic low back pain (CLBP)
- 25 sites randomized 226 patients: At one-year 94/99 (94.9%) of the treatment arm patients and 94/104 (90.3%) of the control arm were available for assessment of outcomes
- ReActiv8 is superior to OMM for the treatment of mechanical chronic low back pain associated with multifidus muscle dysfunction
- Clinically and statistically significant improvements in:
- Disability (Oswestry Disability Index)
- Low back pain (NRS)
- Health-related Quality of Life (EQ-5D)
- ReActiv8 patient improvements accumulate over time, consistent with the restorative mechanism of action
- The majority of patients treated with OMM derived no benefit or had worsening disability, pain, and health-related quality of life at 1-year
- ReActiv8 should be considered earlier in the care continuum for mechanical CLBP
ReActiv8-B Trial – First ever randomized sham-controlled research in neuromodulation
- 204 participants implanted with ReActiv8 system
- Randomized, sham-controlled, double-blinded
- Completer analysis on 62% patients at 5 years (n=126)
- Intent-to-Treat analysis accounting for 100% patients (n=204) provided with Mixed Model of Repeated Measures imputation
- Patient improvements accumulate over time, consistent with restorative mechanism of action
- Explants for success demonstrate increasing number of patients no longer need treatment to maintain clinical benefit
- ONLY restorative therapy for patients suffering from non-surgical, mechanical CLBP evidenced by multifidus dysfunction
- Data from 261 patients completing 2 year follow up from 3 clinical studies (ReActiv8-B, ReActiv8-C, and PMCF)
- Combination of RCT data and Real World Evidence
- Four equal sized cohorts analyzed based on age range (n=65)
- Statistically significant improvements in disability (ODI) and quality of life (EQ-5D-5L) were seen at all assessment time points compared to baseline.
- Consistent improvements in pain (VAS/NRS) at all time points compared to baseline.
- Patients derived significant and clinically meaningful benefit in disability, health related quality of life, and pain, irrespective of age.
- 77% of participants had ≥50% VAS reduction
- 67% reported CLBP resolution (VAS ≤ 2.5 cm)
- 63% had a reduction in ODI of ≥20 points
- Trajectory and durability of three year clinical benefits are consistent with restoration of neuromuscular control and muscle rehabilitation.
ReActiv8-A Trial for CE Mark
- 73% of Completers showed improvement ≥2 points on NRS
- 76% of Completers showed improvement ≥10 points on ODI
- 97% of Completers were very satisfied with treatment
- In participants with disabling intractable CLBP who receive long-term restorative neurostimulation, treatment satisfaction and results remain durable through four years.
Real World Evidence
- 57% of patients experienced a substantial improvement of ≥ 50% reduction in NRS pain score
- 51% of patients experienced a substantial improvement of ≥ 15-point reduction in ODI score
- Excellent safety profile compared to similarly implanted devices
- Single surgeon, single center, real world evidence with one-year clinical follow-up
- 44 patients from the ReActiv8-C study were consecutively included into this cohort if they presented with back pain (NRS) ≥6 and no prior lumbar surgery
- 40 patients completed all required testing at the follow up visit showing statistically significant improvements in pain (NRS), disability (ODI) and quality of life (EQ-5D-5L)
- Response to ReActiv8 is durable and the benefits accumulate over time consistent with the restorative mechanism of action
- No lead migrations
- Results of this real-world experience are consistent with the published data from the earlier ReActiv8-A and ReActiv8-B studies
- 3-year real-world data collected at 5 sites across the UK. 42 patients enrolled w/33 completing 3-year follow up.
- No formal inclusion or exclusion criteria enforced outside the IFU and indications of the CE Mark.
- 70% of patients reached the remitter threshold reporting mild to negligible pain (NRS ≤ 3) and 55% improved by more than 15 points on ODI.
- 75% of patients had a substantial or profound improvement in NRS (>50%) and/or ODI (>20 point). Patients reported a mean EQ-5D approaching an age matched UK population normal value.
- No lead migrations.
- Response to ReActiv8 consistent with the restorative mechanism of action and published pivotal trial data.
Restorative Neurostimulation –
Literature and scientific discussions on the importance of this new therapy
- Re-establishing control of the multifidus muscle may not be feasible with physical therapy and exercise alone.
- Direct electrical stimulation of the multifidus may be a suitable alternative for motor dysfunction.
- A combination of history, imaging, and multiple provocative maneuvers has allowed for increased accuracy in diagnosis, leading to excellent outcomes.
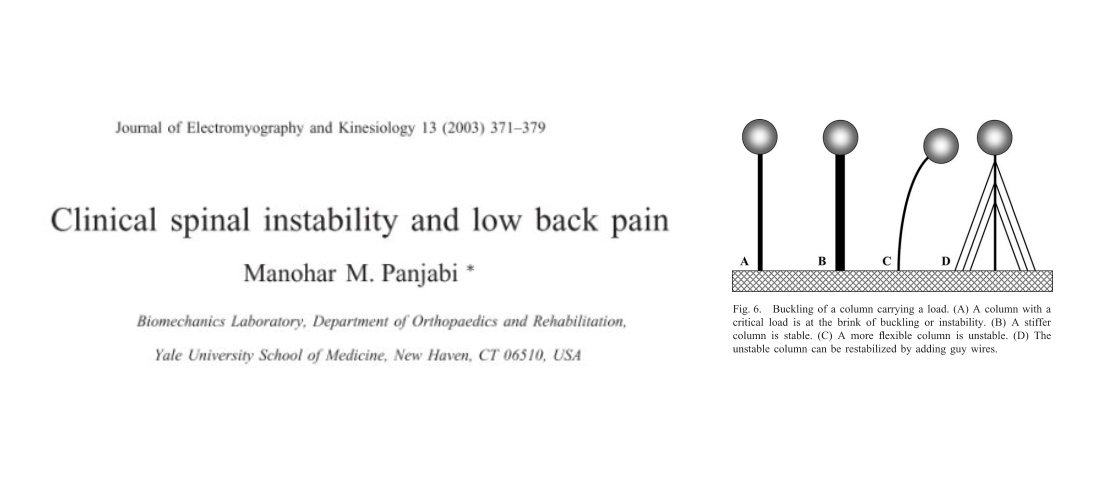
- Clinical instability is related to chronic low back pain.
- Altered motor control and inhibition of the multifidus is a cause of clinical instability and CLBP.
- Back pain due to disrupted muscle control is associated with neuroplastic changes in the motor cortex, which can be reversed with elimination of back pain.
- A program of biofeedback guided motor control exercise of the multifidus can restore some disrupted motor control, but traditional physiotherapy may be very difficult in the context of inhibition.

- First literature review focused on restorative neurostimulation, and the scientific background of the underlying problem being treated.
- Restorative neurostimulation is the first and only PNS device to treat CLBP associated with multifidus dysfunction and loss of neuromuscular control resulting in functional lumbar instability.
- Multifidus dysfunction has been proposed to result from loss of neuromuscular control, which may manifest clinically as muscle inhibition resulting in altered movement patterns.
- Overtime, this cycle may result in potential atrophy, degeneration and CLBP.
- Physical exam demonstrates functional lumbar instability, which conceptually differs from other structural etiologies of CLBP (discovertebral pain, facetogenic pain, stenotic pain).
- Restorative neurostimulation, a novel implantable neurostimulator system, stimulates the efferent lumbar medial branch nerve to elicit repetitive multifidus contractions.
- While various treatments exist for CLBP, restorative neurostimulation distinguishes itself from traditional neurostimulation in a way that treats a different etiology, targets a different anatomical site, and has a distinctive mechanism of action.

- CLBP is a widespread and disabling condition that affects physical, psychological, and social functioning, significantly reducing quality of life. It imposes substantial financial burdens on healthcare systems and society, with costs running into billions annually.
- Despite various non-surgical treatments like medications, exercise, and psychological therapies, CLBP remains difficult to manage effectively. The condition often persists due to factors like muscle dysfunction and the complexity of pain mechanisms.
- Recent advancements include the use of multifidus neurostimulation devices, which have shown promising results in reducing pain and improving function in patients with mechanical CLBP. These devices help restore muscle control and stability, offering a new avenue for treatment.
Physical Testing –
How to objectively identify patients with neuromotor dysfunction

- Observation of trunk movement is considered an important part of the clinical examination of patients with low back pain (LBP).
- The presence of forward-bending movement aberrance is frequently seen in patients with acute/subacute, nonspecific LBP, compared to those without a history of LBP.
- Aberrant movements indicate that some motor control or musculoskeletal impairment remains unresolved in this group.
- The lumbar multifidus muscle is a critical contributor to lumbar spine stability and deficits in its function are associated with LBP.
- A physical examination method assessing multifidus function could provide great clinical utility as a diagnostic approach.
- Results provide evidence supporting the reliability and validity of the Multifidus Lift Test (MLT) to assess lumbar multifidus function.
- Clinical or functional instability consists of insufficient motor control and is a factor in abnormal inter-segmental movement and LBP, where no lumbar architecture defect can be observed on imaging.
- In the absence of imaging as a tool, reliable physical assessments are critical for proper diagnosis of functional instability.
- The prone instability test (PIT) demonstrates good reliability and moderate accuracy in diagnosing functional lumbar instability.
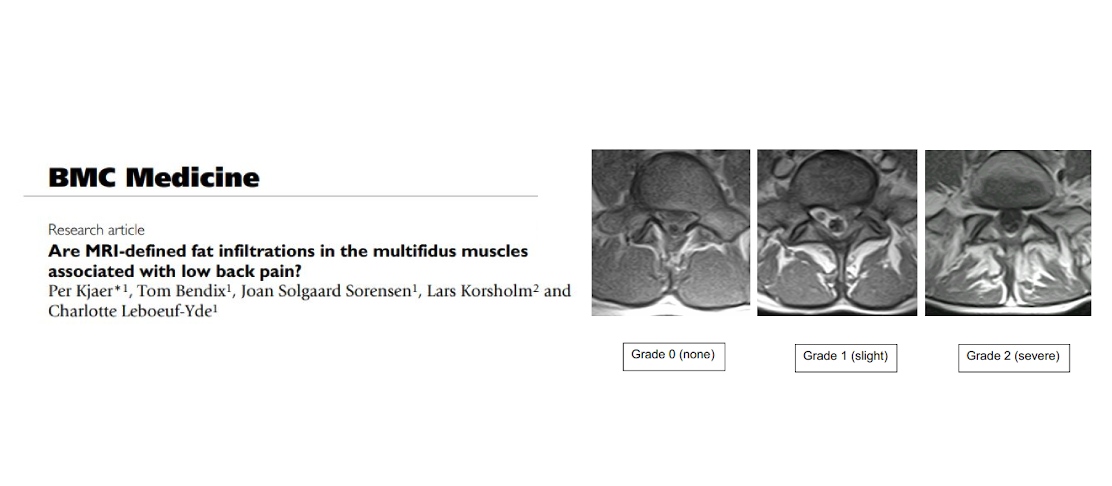
Role of the multifidus – how recent science has identified
this muscle as critical in preventing CLBP
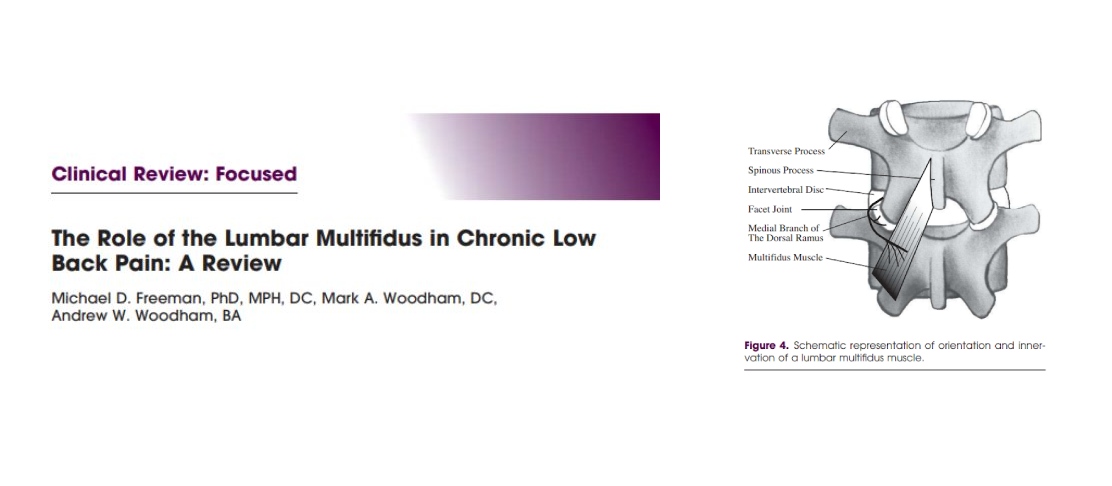
- The Multifidus morphology is uniquely different from other lumbar muscles, and therefore has a special role in lumbar stability.
- Changes in the multifidus have been found by many studies to be related to low back pain.
- Injury and overloading of lumbar tissues has been shown to cause multifidus inhibition.
- Clinical studies have demonstrated that the multifidus can be rehabilitated and low back pain decreased.

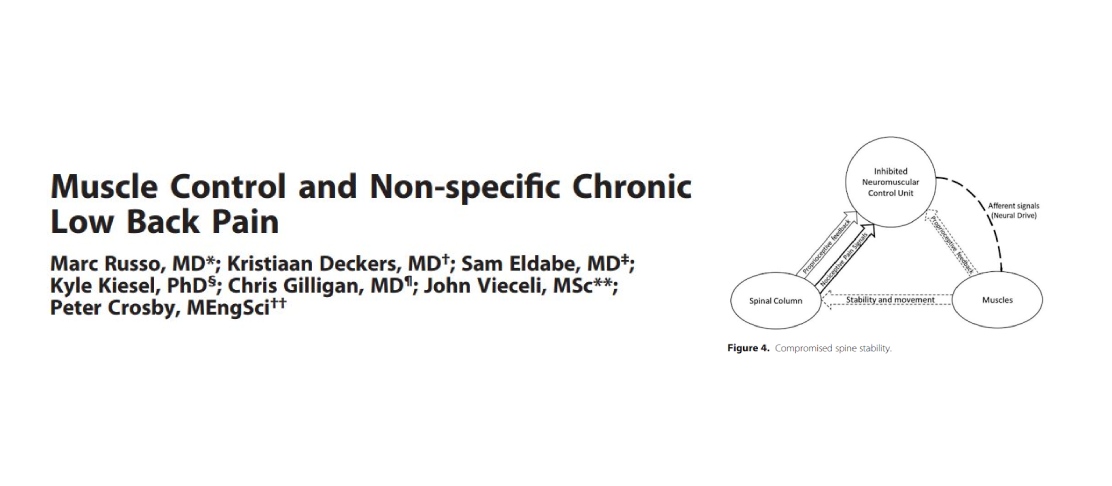
- The spinal stabilizing system consists of three subsystems:
- the passive spinal column subsystem,
- the active muscular subsystem,
- the neural and feedback control subsystem.
- Injury, degeneration or disease can cause dysfunction in the spinal system, which cannot be compensated for beyond certain limits.
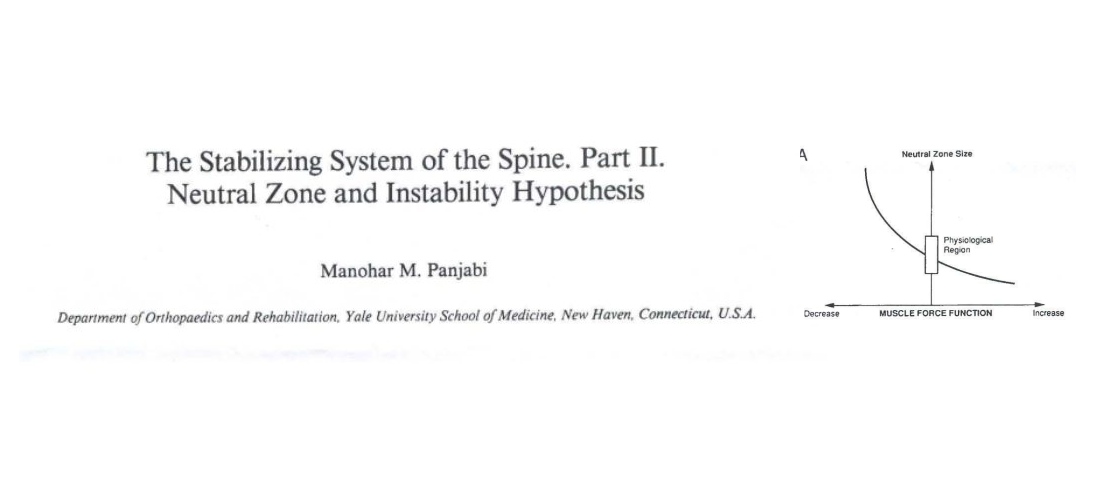
- The neutral zone is the spinal range of motion where there is little to no resistance.
- An increase in the size of the neutral zone is correlated with spinal degeneration and injury.
- The bodies’ inability to maintain neutral zones within physiological limits, therefore causing mechanical dysfunction and pain, is termed “clinical instability”.
- Improved neurocontrol and motor function may reduce an aberrant neutral zone, decreasing clinical instability and reducing pain.
- Increased neutral zones as a result of injury or degeneration are shown to be correlated to pain.
- The spinal muscles provide significant stability to the spine.
- Less efficient muscular control and decreased stability has been found in patients with low back pain.
- A compromised spinal system can be stabilized with muscle strengthening and retraining of the neuromuscular control system.
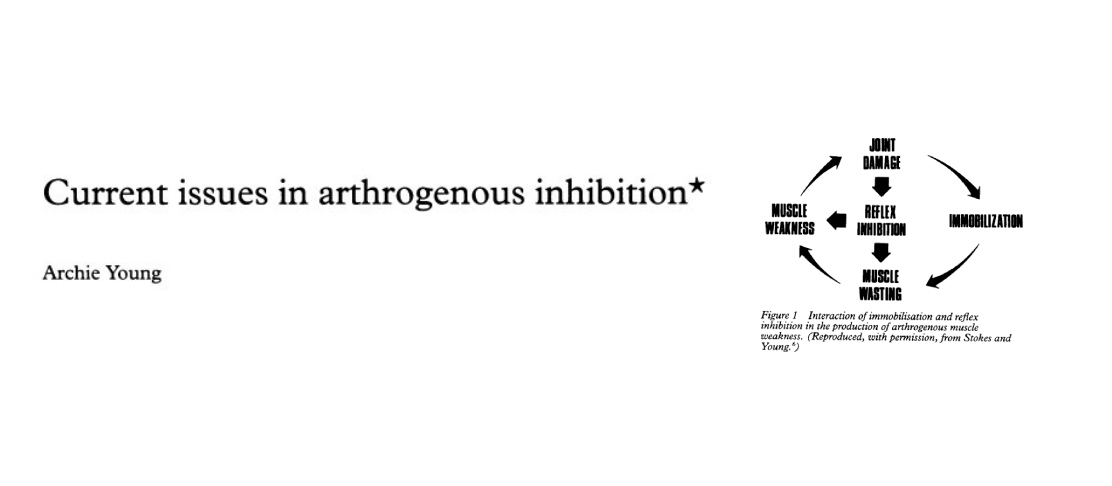
- Inhibition produces underlying weakness in muscles associated with joint disease, and studies suggest possible neurophysiological mechanisms are involved.
- Severe motor inhibition limits the potential response to voluntary therapeutic exercise.
- Studies of intermittent neurostimulation of motor neurons in patients showed no evidence of the atrophy in type I and type II muscle fibers seen in untreated patients.
Society Guidelines and Support
- The highest-level trial of the permanently implanted PNS system was an international, multi-center, prospective, randomized, active, sham controlled, blinded trial, which generated high, level I-A evidence supporting the significance of the treatment effect.
- The ReActiv8-B trial “demonstrated clinical effectiveness as measured by substantial and durable improvements in pain, disability, and quality of life in a cohort of patients with a favorable benefit risk profile.
- The rates of adverse events are consistent with known SAE rates for spinal cord stimulation therapy; however, there was no finding of lead migration.
- The ASPN Back Group recommends offering the permanently implanted PNS system given that there is high certainty that the net benefit is substantial.
- Restorative neurostimulation for CLBP is supported by several clinical studies that show robust and durable clinical effects over the pretreatment condition.
- The totality of evidence suggests that in a well-selected patient population who have exhausted conventional care paradigms, the potential benefits outweigh the risks and costs.
- These patients tend to be exposed to multiple therapies with limited durability, resulting in a continuous cycle of high-cost health care utilization.
- Restorative neurostimulation should be considered for clinically appropriate patients who have exhausted reasonable conservative approaches.
Healthcare Economics
- In addition to clinically meaningful improvements in pain and function with long term durability, the overwhelming majority of patients transitioned from a high to a low-impact CLBP state.
- 71% of patients had High Impact pain at baseline that reduced to 10% at 2 years
- 85% of patients reported low-impact pain at 2 years
- This is typically associated with significantly lower direct and indirect healthcare utilization levels.
- The recovery trajectory is consistent with a restorative mechanism of action and suggests that over the long term these health states will be maintained.
MRI Conditionality (US FDA Clearance Only)
- FDA Approval for MRI Labeling on ReActiv8® Restorative Neurostimulation System™